Lower Urinary Tract Obstruction (LUTO)
or Bladder Outlet Obstruction (BOO)
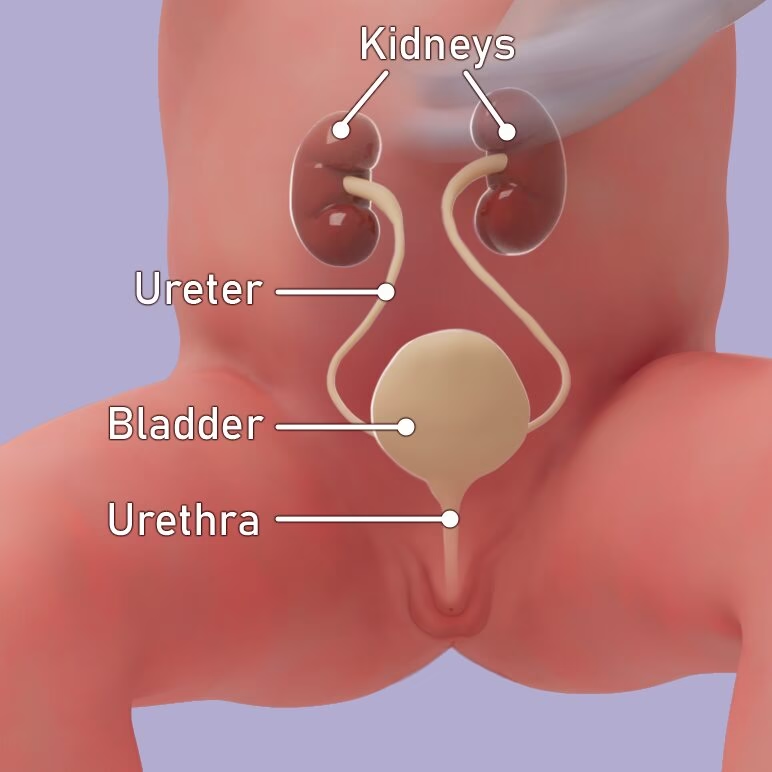
Normal Anatomy
The urinary tract is made up of organs that produce and store urine, or pee. It includes:
- Two kidneys
- Two ureters
- The bladder
- And the urethra.
The kidneys make the urine, which flows through the ureters into the bladder, where it is stored. When the bladder is full, it pushes the urine out through the urethra.
The kidneys and ureters are called the upper urinary tract and the bladder and urethra the lower urinary tract.
In the uterus, or womb, the urine is called amniotic fluid, and it cushions the fetus.
Lower Urinary Tract Obstruction (LUTO)
What happened?
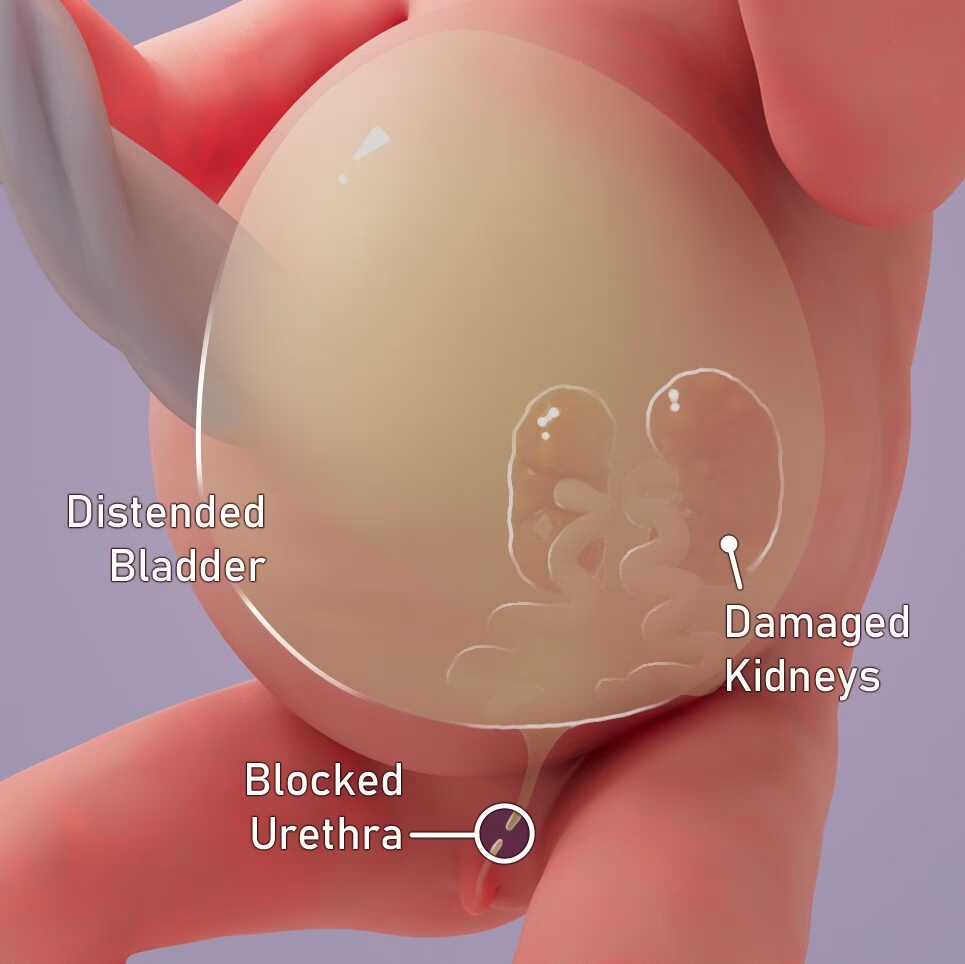
LUTO happens when the urethra is blocked, and urine can’t flow out of the body. This causes urine to build up in the kidneys and ureters. Over time, this can harm the kidneys.
While the fetus is in the womb, the placenta acts as both lungs and kidneys. But after birth, the baby can’t rely on the placenta anymore, and the lungs and kidneys must begin functioning on their own.
If LUTO has caused damage to the baby’s organs, they may not work properly which can affect the baby’s health and lower the chance of survival.
Causes of LUTO
LUTO can happen because of a problem the baby’s genetics, or it can happen for no known reason (“isolated” LUTO). Whether genetic or isolated, LUTO is caused by a structural issue with the urethra. After birth, doctors can run tests to find out exactly why LUTO happened, which helps them decide how to treat the baby.
The most common structure anomalies are:
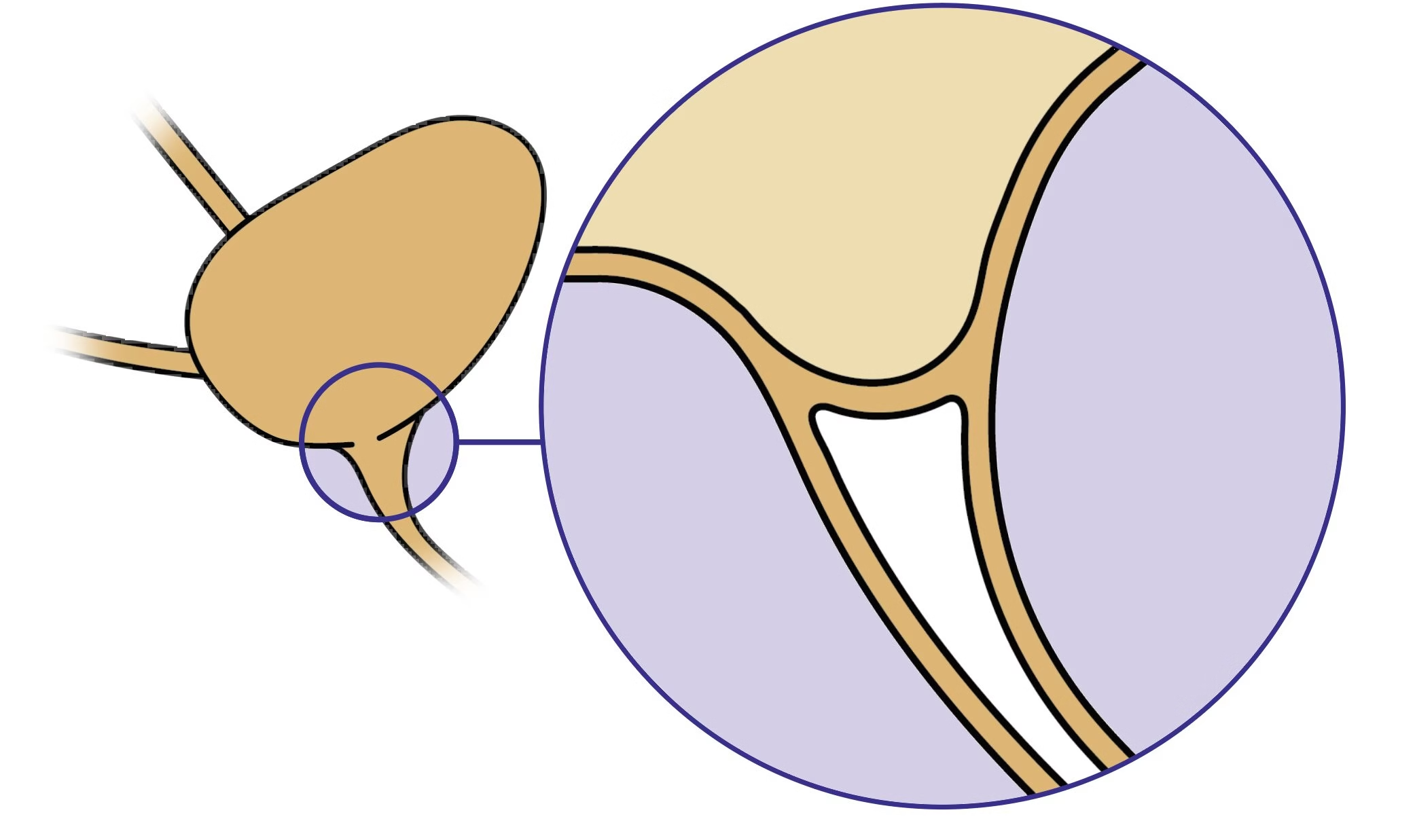
Posterior Urethral Valve
Complete Obstruction
This is where a fold of tissue blocks the urethra, stopping urine from leaving the body.
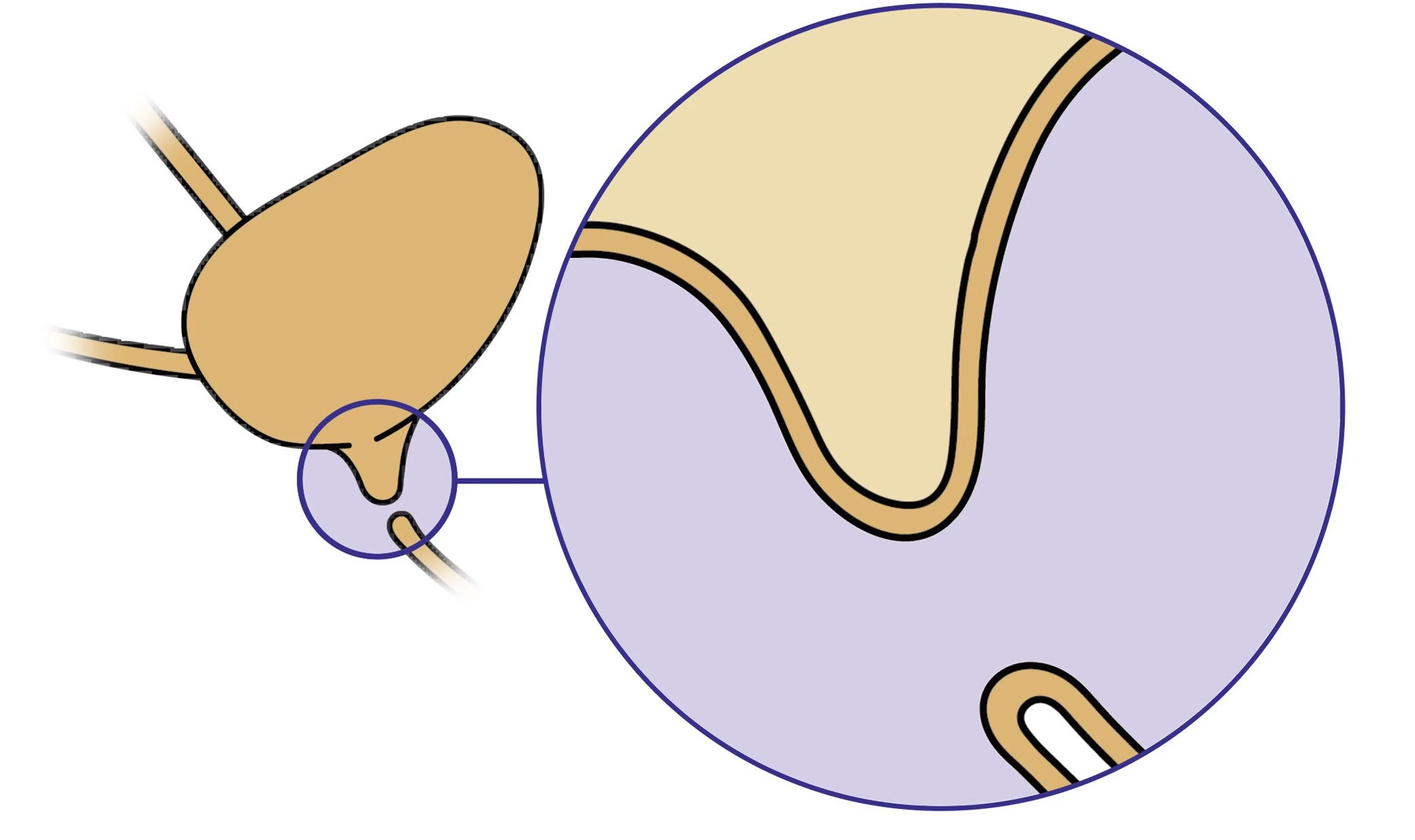
Urethral Atresia
Complete Obstruction
This is where the urethra is absent, stopping the flow of urine.
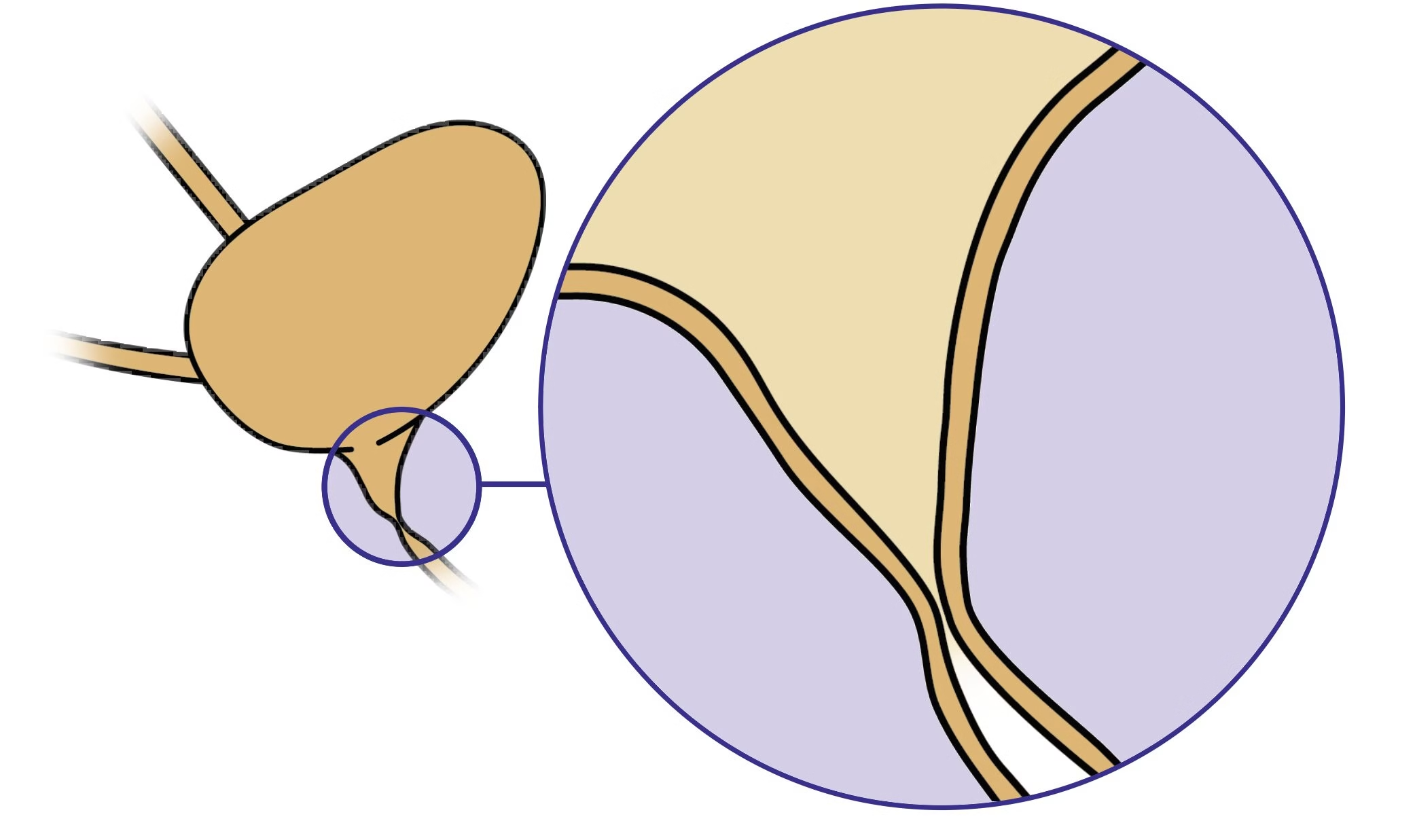
Urethral Stricture
Partial Obstruction
This is where parts of the urethra are narrowed, restricting the flow of urine.
How LUTO is Diagnosed
Doctors use several tests to find out if a fetus has LUTO. These tests include:

Ultrasound
This test uses sound waves to make pictures of the fetus inside of the womb. It helps doctors check the baby’s organs, to look for any problems, and monitor growth.
MRI
This test makes images of the fetal body strong magnets. MRI helps doctors look closely at certain areas, like the fetal urinary tract.

Fetal Echocardiography
This test looks at the fetal heart to check for any malformations, as babies with birth defects such as LUTO are at higher risk for heart issues.

Amniocentesis
In this test, doctors take a small sample the amniotic fluid surrounding the baby. They can check the cells in this fluid for genetic problems or conditions.
Fetal Urinary Electrolytes
This test checks how well the baby’s kidneys are working by draining urine from the bladder to test it.
Impact on Development
When the urethra is blocked, the baby can’t urinate, which affects other parts of the body.
Kidneys
When urine builds up, it can damage the kidneys.
This can cause hydronephrosis, or very swollen kidneys, which can lead to kidney failure .
It can also cause multicystic dysplastic kidneys, which means the kidneys don’t grow properly and are filled with fluid instead of normal kidney tissue.
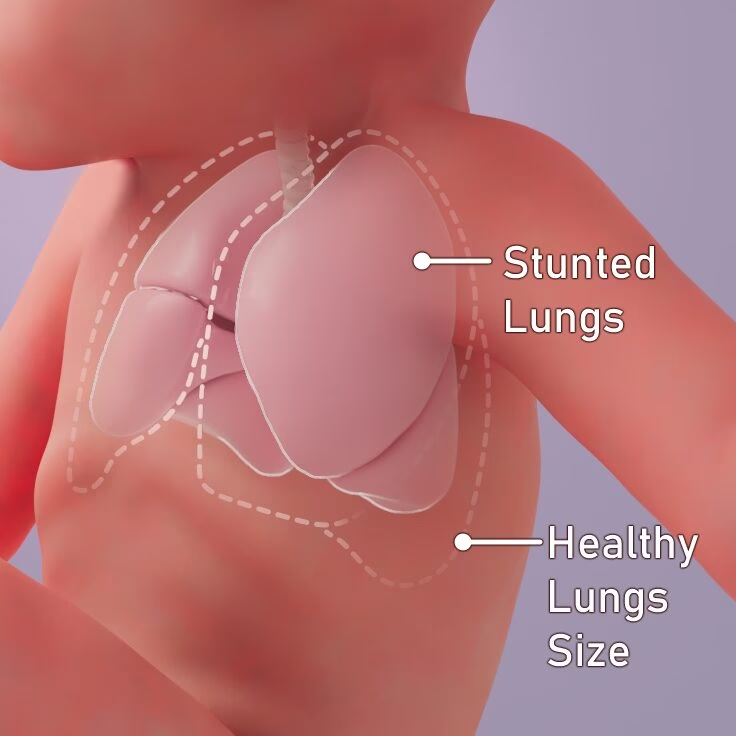
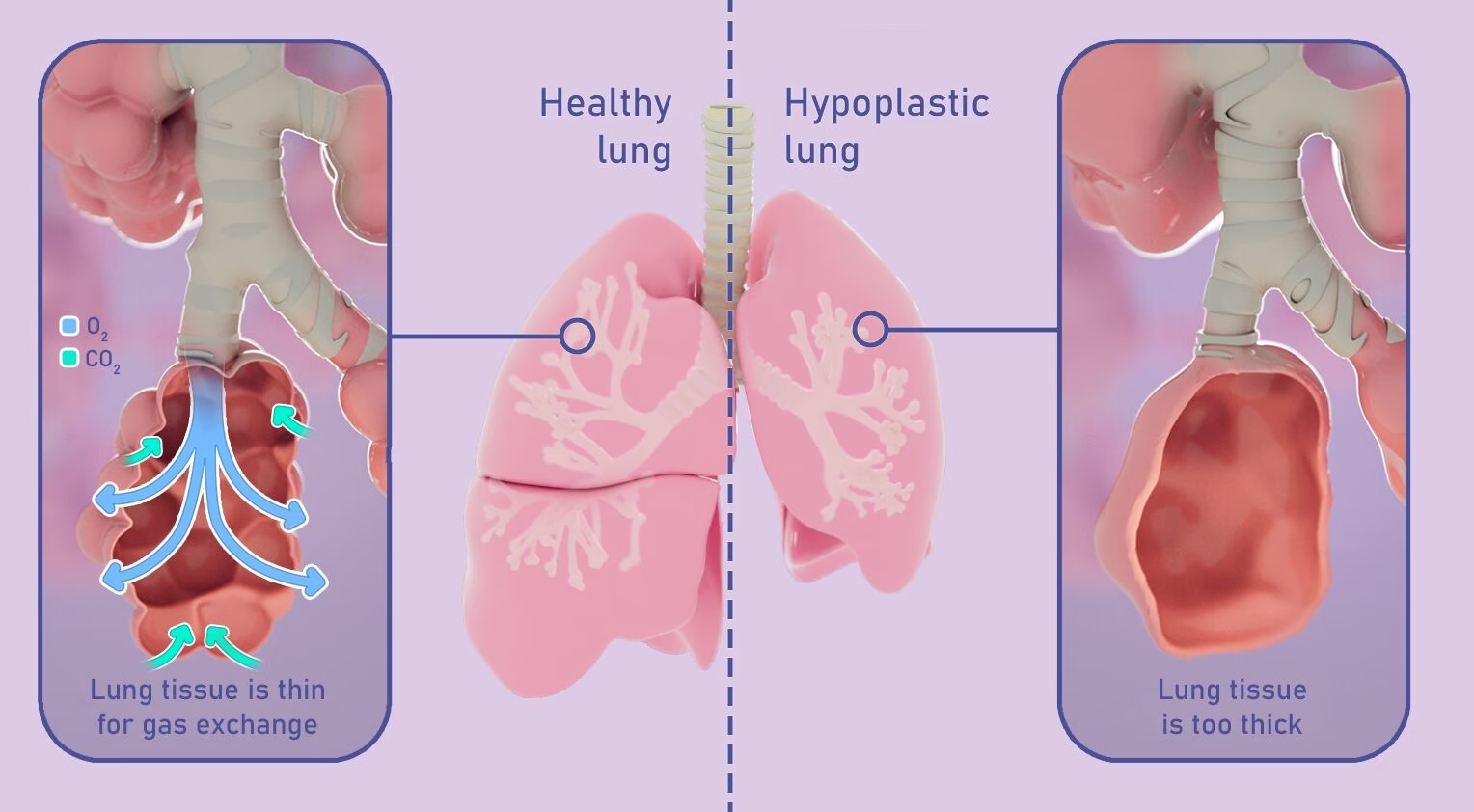
Lungs
Normally, the baby “breathes” in amniotic fluid, which helps the lungs grow, like filling a water balloon. But when the baby can’t release urine, there isn’t enough amniotic fluid to help the lungs grow.
This may lead to hypoplastic lungs, meaning the lungs are undeveloped and can’t work properly after birth .
Physical Issues
Amniotic fluid cushions the fetus in the womb, giving it space to move around. Without enough fluid, there is less room for the fetus, which can cause problems like facial deformities (“Potter facies“), short limbs, clubbed feet, and joint contractions (where the joints can’t move properly).
These physical defects are knowns as Potter syndrome.
The outlook for babies with LUTO depends on how serious the blockage is and how badly other organs, like the kidneys or lungs, are affected.
Some babies may need treatments like a ventilator, dialysis, or even a kidney transplant after birth. Babies with severe LUTO have a lower chance of surviving, and even if they do survive birth, they may still need a lot of medical support.
Intervention Options
There are interventions that can help some babies with LUTO, but they don’t fix everything, and the baby will likely still have kidney or lung damage. Doctors use many tests to decide if these interventions will help.
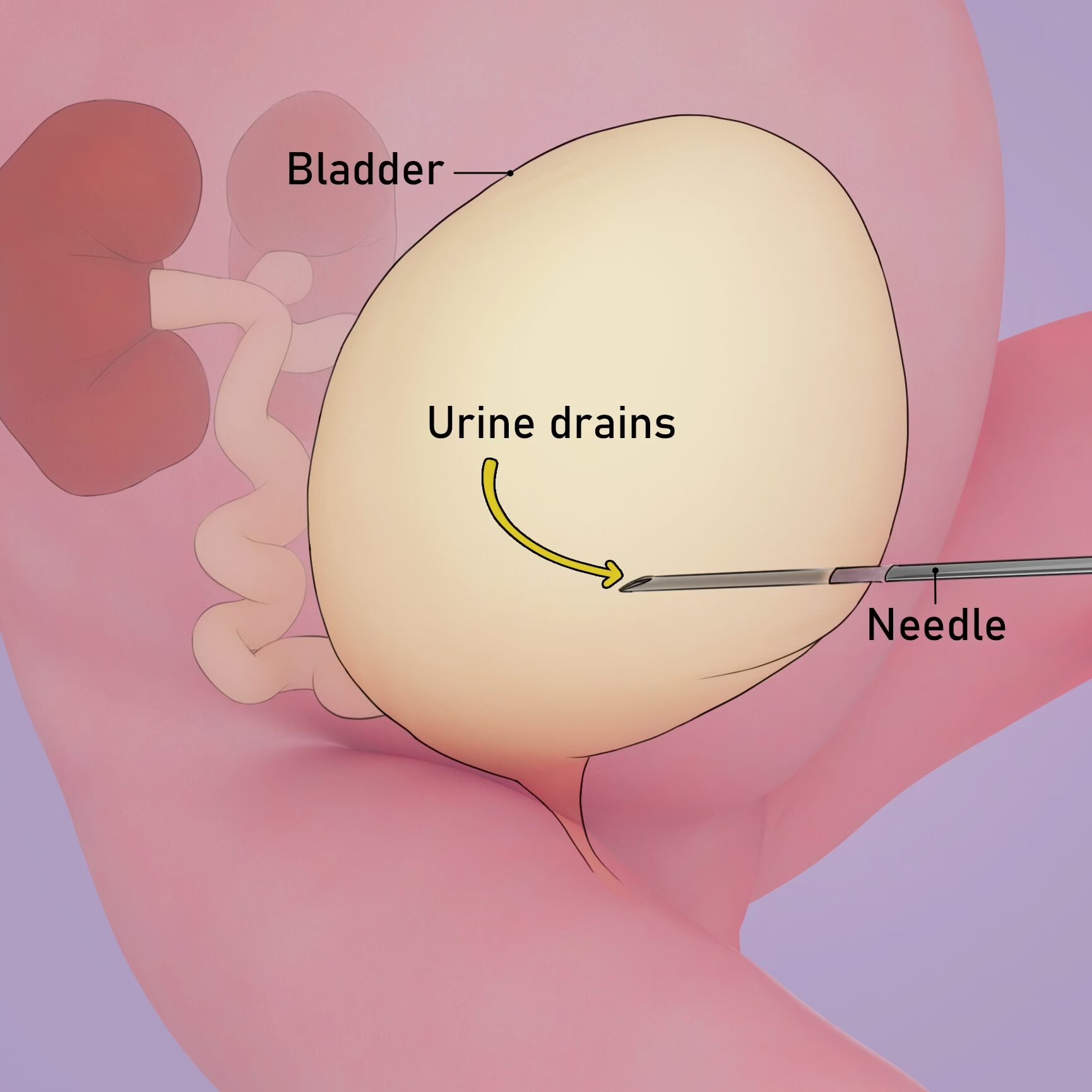
Vesicocentesis
This is a temporary measure where a needle is used to take urine out of the baby’s bladder. This helps relieve pressure. This may need to be repeated several times throughout the pregnancy.
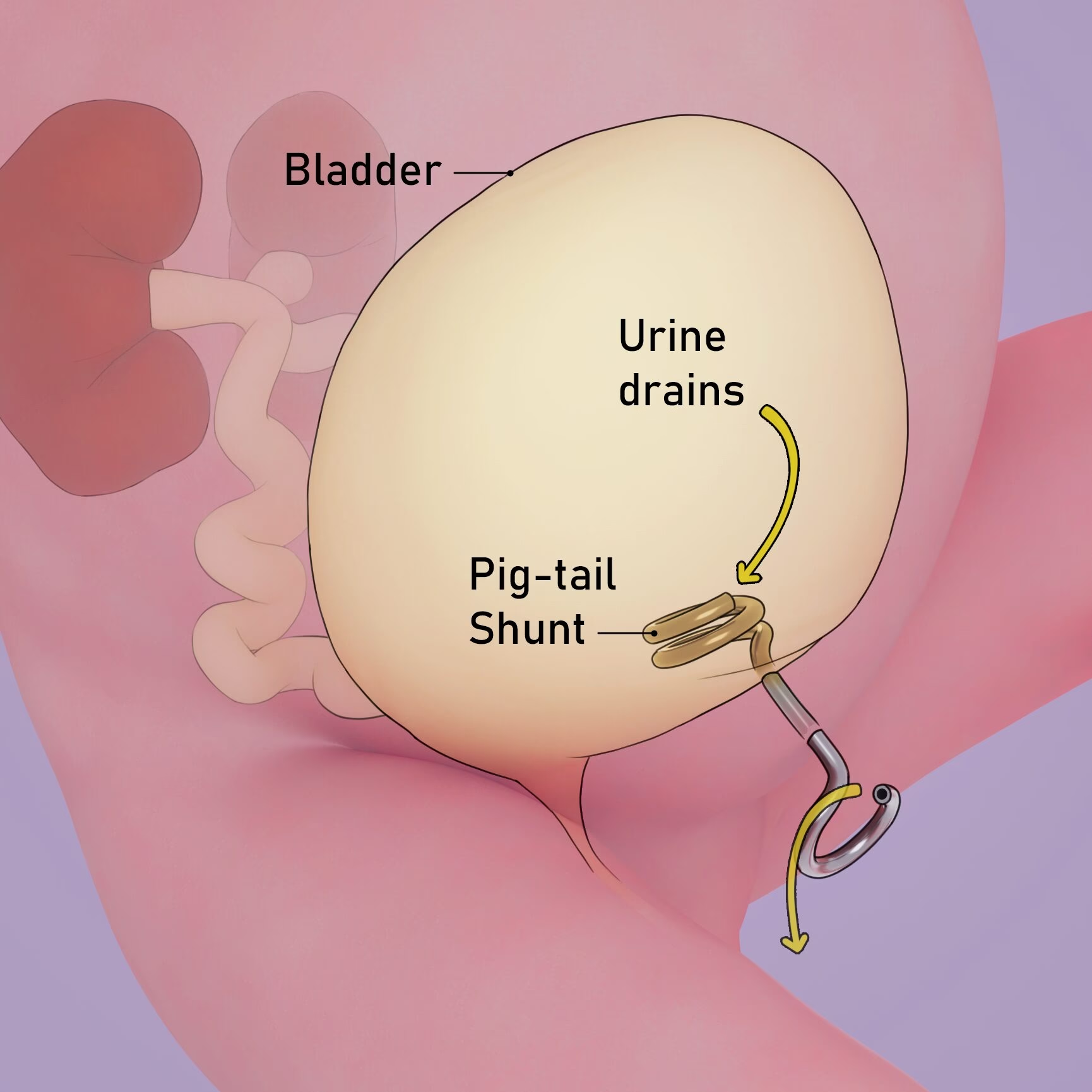
Pigtail Shunt
A shunt is a small tube that is put into the baby’s bladder through the womb. The tube helps the fluid drain into the amniotic space, which can reduce the build-up of urine. This is a temporary measure until the baby is born.
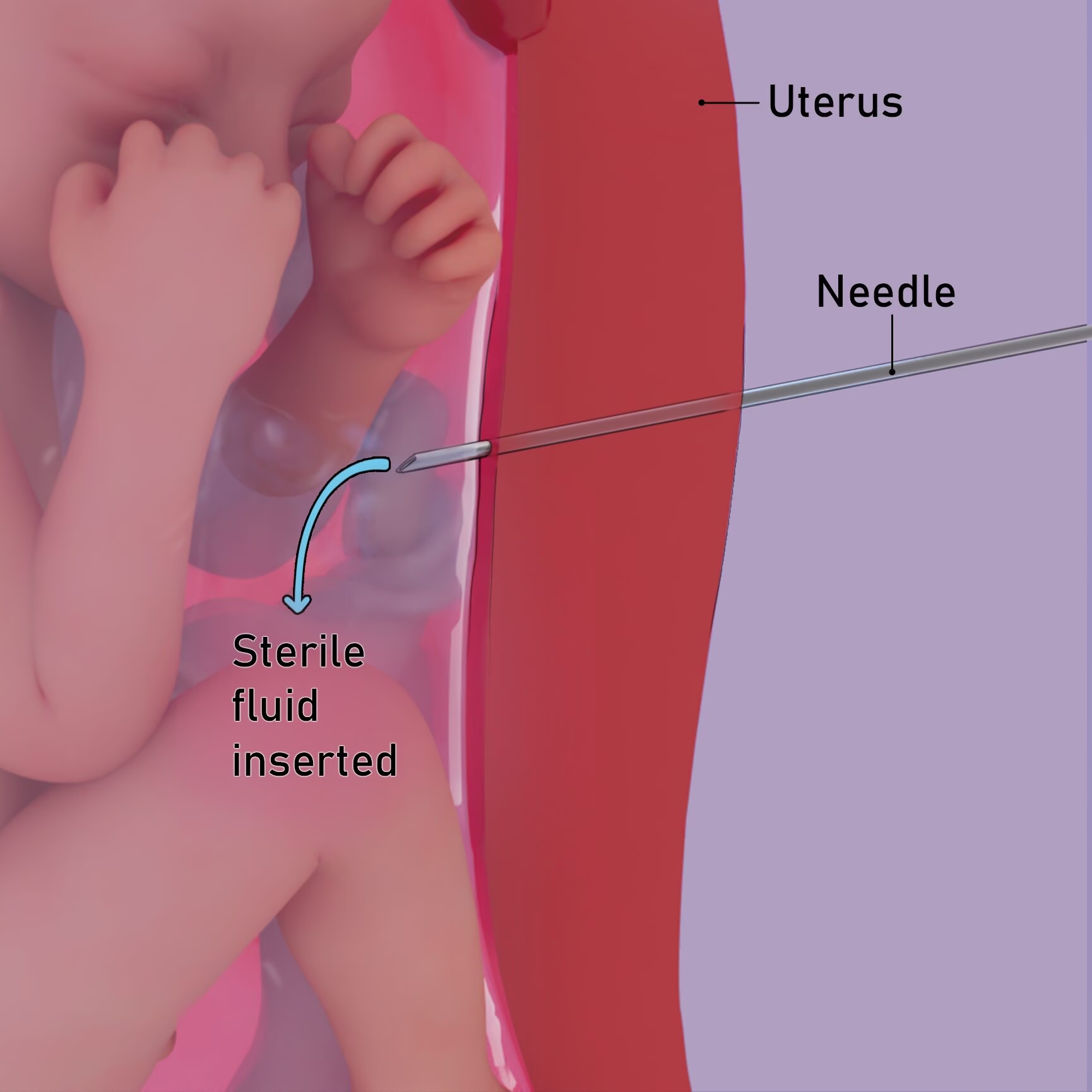
Amnioinfusion
In this procedure, a needle is used to put sterile fluid into the uterus to help cushion the fetus and help the lungs to grow better. This may need to be repeated several times throughout the pregnancy.
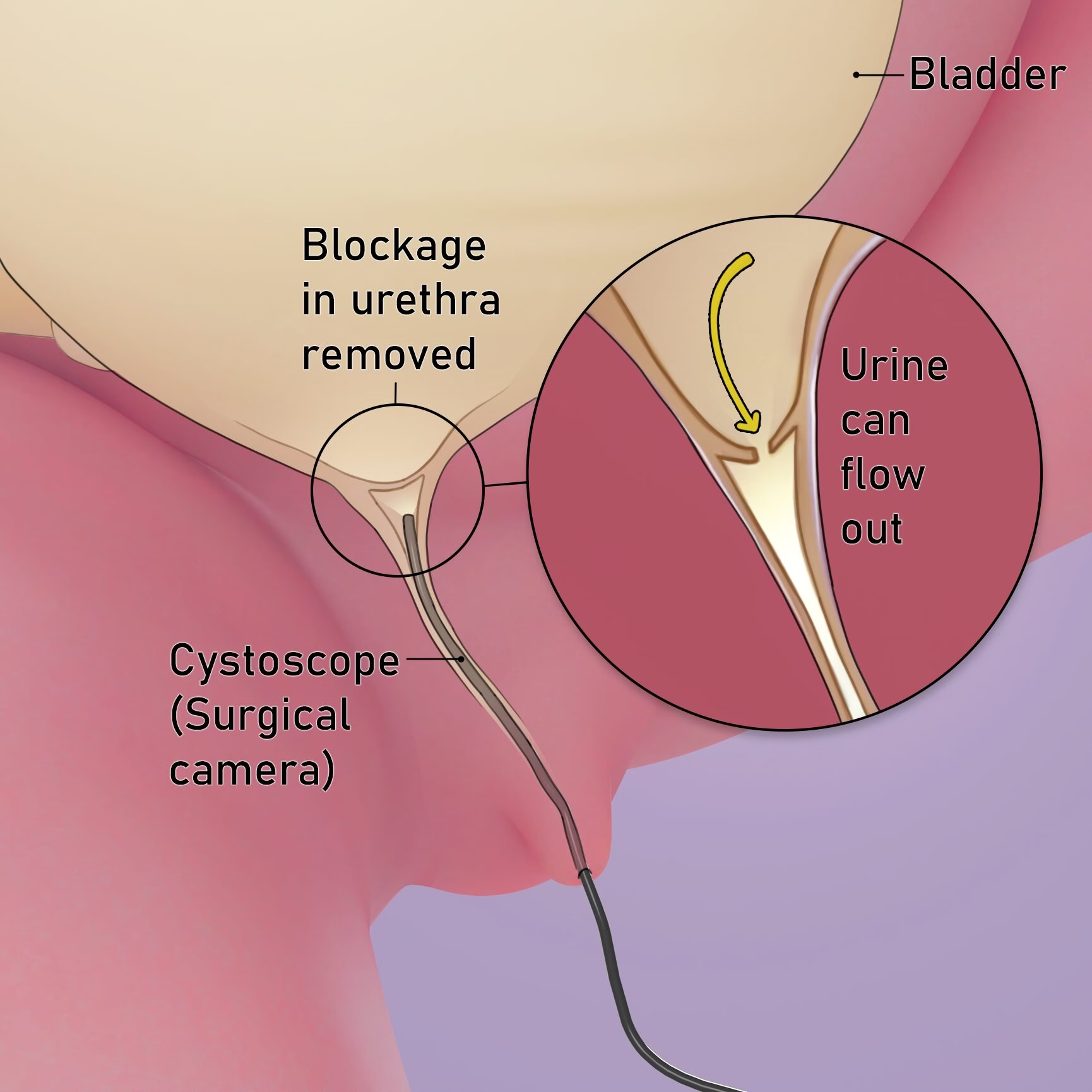
Fetal Cystoscopy
In rare cases, doctors can perform a small surgery on the fetus using a cystoscope (small, surgical camera) to remove the blockage in the fetal urethra.
Resources
Essential Information on LUTO - Printable Summary
File Type: PDF
File Size: 230 kb
Pages: 2
Print this Webpage
File Type: PDF
File Size: 1.3 MB
Pages: 5
About my Thesis:
Accessible Education for LUTO Patients: A Study of Multimodal Tools to Support Literacy and Emotional Wellbeing
Year
2025
Thesis Committee
Michelle Kush, MD
Thesis Preceptor
Jennifer Fairman, CMI
Thesis Advisor
Format
3D Animation, Website, Patient Handout, 3D Prints
Objectives:
with foundational knowledge.
Facilitate communication by developing online materials that empower patients to explain their condition to family and friends, reducing the need for repeated explanations.
Support patient education by providing educational materials to healthcare providers.
Tools
ZBrush, Cinema4D, RedShift, AfterEffects, Illustrator, Photoshop, InDesign
Links and Resources
LUTO - Patient Education
LUTO - Research Articles
LUTO:
Capone, V., Persico, N., Berrettini, A., Decramer, S., De Marco, E. A., De Palma, D., Familiari, A., Feitz, W., Herthelius, M., Kazlauskas, V., Liebau, M., Manzoni, G., Maternik, M., Mosiello, G., Schanstra, J. P., Vande Walle, J., Wühl, E., Ylinen, E., Zurowska, A., Montini, G. (2022). Definition, diagnosis and management of fetal lower urinary tract obstruction: Consensus of the ERKNet CAKUT-Obstructive Uropathy Work Group. Nature Reviews Urology, 19(5), 295–303. https://doi.org/10.1038/s41585-022-00563-8
Haeri, S. (2015). Fetal Lower Urinary Tract Obstruction (LUTO): A practical review for providers. Maternal Health, Neonatology and Perinatology, 1, 26. https://doi.org/10.1186/s40748-015-0026-1
Kohl, T. (2022). Management of very young fetuses with LUTO. Nature Reviews Urology, 19(10), 627–628. https://doi.org/10.1038/s41585-022-00636-8
Malin, G., Tonks, A., Morris, R., Gardosi, J., & Kilby, M. (2012). Congenital lower urinary tract obstruction: A population-based epidemiological study. BJOG: An International Journal of Obstetrics & Gynaecology, 119(12), 1455–1464. https://doi.org/10.1111/j.1471-0528.2012.03476.x
Mandaletti, M., Cerchia, E., Ruggiero, E., Teruzzi, E., Bastonero, S., Pertusio, A., Della Corte, M., Sciarrone, A., & Gerocarni Nappo, S. (2024). Obstructive or non-obstructive megacystis: A prenatal dilemma. Frontiers in Pediatrics, 12, 1379267. https://doi.org/10.3389/fped.2024.1379267
Morris, R. K., & Kilby, M. D. (2011). Long-term renal and neurodevelopmental outcome in infants with LUTO, with and without fetal intervention. Early Human Development, 87(9), 607–610. https://doi.org/10.1016/j.earlhumdev.2011.07.004
Ruano, R., Dunn, T., Braun, M. C., Angelo, J. R., & Safdar, A. (2017). Lower urinary tract obstruction: Fetal intervention based on prenatal staging. Pediatric Nephrology, 32(10), 1871–1878. https://doi.org/10.1007/s00467-017-3593-8
Lung Development:
Fitzsimmons, E. D., & Bajaj, T. (2025). Embryology, Amniotic Fluid. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK541089/
Hooper, S. B., & Harding, R. (1995). FETAL LUNG LIQUID: A MAJOR DETERMINANT OF THE GROWTH AND FUNCTIONAL DEVELOPMENT OF THE FETAL LUNG. Clinical and Experimental Pharmacology and Physiology, 22(4), 235–241. https://doi.org/10.1111/j.1440-1681.1995.tb01988.x
Schittny, J. C. (2017). Development of the lung. Cell and Tissue Research, 367(3), 427–444. https://doi.org/10.1007/s00441-016-2545-0
Associated Diseases in Fetuses and Infants:
Bhandari, J., Thada, P. K., & Sergent, S. R. (2025). Potter Syndrome. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK560858/
Klaus, R., & Lange-Sperandio, B. (2022). Chronic Kidney Disease in Boys with Posterior Urethral Valves–Pathogenesis, Prognosis and Management. Biomedicines, 10(8), 1894. https://doi.org/10.3390/biomedicines10081894
Multimedia Learning
Importance of Health Literacy in Health Care:
Alshaikh, L., Shimozono, Y., Dankert, J. F., Ubillus, H., & Kennedy, J. G. (2021). Evaluation of the Quality and Readability of Online Sources on the Diagnosis and Management of Osteochondral Lesions of the Ankle. CARTILAGE, 13(1_suppl), 1422S-1428S. https://doi.org/10.1177/19476035211021910
Knudsen, B. M., Søndergaard, S. R., Stacey, D., & Steffensen, K. D. (2024). Impact of timing and format of patient decision aids for breast cancer patients on their involvement in and preparedness for decision making—The IMPACTT randomised controlled trial protocol. BMC Cancer, 24(1), 336. https://doi.org/10.1186/s12885-024-12086-z
Kraft, S. A., Constantine, M., Magnus, D., Porter, K. M., Lee, S. S.-J., Green, M., Kass, N. E., Wilfond, B. S., & Cho, M. K. (2017). A randomized study of multimedia informational aids for research on medical practices: Implications for informed consent. Clinical Trials, 14(1), 94–102. https://doi.org/10.1177/1740774516669352
Lindau, S. T., Tomori, C., Lyons, T., Langseth, L., Bennett, C. L., & Garcia, P. (2002). The association of health literacy with cervical cancer prevention knowledge and health behaviors in a multiethnic cohort of women. American Journal of Obstetrics and Gynecology, 186(5), 938–943. https://doi.org/10.1067/mob.2002.122091
Marteau, T. M., Kidd, J., Cuddeford, L., & Walker, P. (1996). Reducing anxiety in women referred for colposcopy using an information booklet. British Journal of Health Psychology, 1(2), 181–189. https://doi.org/10.1111/j.2044-8287.1996.tb00501.x
Menendez, M. E., Van Hoorn, B. T., Mackert, M., Donovan, E. E., Chen, N. C., & Ring, D. (2017). Patients With Limited Health Literacy Ask Fewer Questions During Office Visits With Hand Surgeons. Clinical Orthopaedics & Related Research, 475(5), 1291–1297. https://doi.org/10.1007/s11999-016-5140-5
Patterson, C., & Teale, C. (1997). Influence of written information on patients’ knowledge of their diagnosis. Age and Ageing, 26(1), 41–42. https://doi.org/10.1093/ageing/26.1.41
Ragsdale, L. B. (2020). Why Is Everyone Giving up on Our Son? In L. B. Ragsdale & E. G. Miller (Eds.), Pediatric Palliative Care (pp. 7–12). Oxford University Press. https://doi.org/10.1093/med/9780190051853.003.0002
Emotional Impact of Community or Health Literacy during Pregnancy:
Altshuler, A. L., Ojanen-Goldsmith, A., Blumenthal, P. D., & Freedman, L. R. (2021). “Going through it together”: Being accompanied by loved ones during birth and abortion. Social Science & Medicine, 284, 114234. https://doi.org/10.1016/j.socscimed.2021.114234
Department of Gynecology and Obstetrics, İstanbul University, İstanbul, Turkey, Ekinci, G., İnal, S., & Department of Midwifery, İstanbul University-Cerrahpaşa, Faculty of Health Sciences, İstanbul, Turkey. (2024). Evaluation of Effective Factors on Decision of Families Regarding Medical Abortion Recommended due to Fetal Anomaly. Florence Nightingale Journal of Nursing, 32(1), 83–89. https://doi.org/10.5152/FNJN.2024.23007
Jacobs, S., Davies, N., Butterick, K. L., Oswell, J. L., Siapka, K., & Smith, C. H. (2023). Shared decision-making for children with medical complexity in community health services: A scoping review. BMJ Paediatrics Open, 7(1), e001866. https://doi.org/10.1136/bmjpo-2023-001866
Impact of 3D Models:
Bernhard, J.-C., Isotani, S., Matsugasumi, T., Duddalwar, V., Hung, A. J., Suer, E., Baco, E., Satkunasivam, R., Djaladat, H., Metcalfe, C., Hu, B., Wong, K., Park, D., Nguyen, M., Hwang, D., Bazargani, S. T., De Castro Abreu, A. L., Aron, M., Ukimura, O., & Gill, I. S. (2016). Personalized 3D printed model of kidney and tumor anatomy: A useful tool for patient education. World Journal of Urology, 34(3), 337–345. https://doi.org/10.1007/s00345-015-1632-2
Ghazi, A. E., & Teplitz, B. A. (2020). Role of 3D printing in surgical education for robotic urology procedures. Translational Andrology and Urology, 9(2), 93141–93941. https://doi.org/10.21037/tau.2020.01.03
Harris, M. A., Peck, R. F., Colton, S., Morris, J., Chaibub Neto, E., & Kallio, J. (2009). A Combination of Hand-held Models and Computer Imaging Programs Helps Students Answer Oral Questions about Molecular Structure and Function: A Controlled Investigation of Student Learning. CBE—Life Sciences Education, 8(1), 29–43. https://doi.org/10.1187/cbe.08-07-0039
Karsenty, C., Guitarte, A., Dulac, Y., Briot, J., Hascoet, S., Vincent, R., Delepaul, B., Vignaud, P., Djeddai, C., Hadeed, K., & Acar, P. (2021). The usefulness of 3D printed heart models for medical student education in congenital heart disease. BMC Medical Education, 21(1), 480. https://doi.org/10.1186/s12909-021-02917-z
Novak, M., & Schwan, S. (2021). Does Touching Real Objects Affect Learning? Educational Psychology Review, 33(2), 637–665. https://doi.org/10.1007/s10648-020-09551-z
Recker, F., Schremmer, T., Berg, C., Schäfer, V. S., Strizek, B., & Jimenez‐Cruz, J. (2024). Advancement of 3D printing technology for the development of a training model in US ‐guided vesicoamniotic shunting for early LUTO therapy. Acta Obstetricia et Gynecologica Scandinavica, 103(8), 1550–1557. https://doi.org/10.1111/aogs.14879
Impact of Video & Multimedia:
Bush, A. J., & Gresham, L. G. (1986). The communication effects of animation. Journal of Applied Communication Research, 14(1), 59–65. https://doi.org/10.1080/00909888609360303
Choi, S., Ahn, J., Lee, D., & Jung, Y. (2009). The Effectiveness of Mobile Discharge Instruction Videos (MDIVs) in Communicating Discharge Instructions to Patients with Lacerations or Sprains: Southern Medical Journal, 102(3), 239–247. https://doi.org/10.1097/SMJ.0b013e318197f319
Deshpande, N., Wu, M., Kelly, C., Woodrick, N., Werner, D. A., Volerman, A., & Press, V. G. (2023). Video-Based Educational Interventions for Patients With Chronic Illnesses: Systematic Review. Journal of Medical Internet Research, 25, e41092. https://doi.org/10.2196/41092
Feeley, T. H., Keller, M., & Kayler, L. (2023). Using Animated Videos to Increase Patient Knowledge: A Meta-Analytic Review. Health Education & Behavior: The Official Publication of the Society for Public Health Education, 50(2), 240–249. https://doi.org/10.1177/10901981221116791
Fiore-Silfvast, B., Hartung, C., Iyengar, K., Iyengar, S., Israel-Ballard, K., Perin, N., & Anderson, R. (2013). Mobile video for patient education: The midwives’ perspective. Proceedings of the 3rd ACM Symposium on Computing for Development, 1–10. https://doi.org/10.1145/2442882.2442885
Gagliano, M. E. (1988). A literature review on the efficacy of video in patient education: Academic Medicine, 63(10), 785–792. https://doi.org/10.1097/00001888-198810000-00006
Leiner, M. (2004). Patient communication: A multidisciplinary approach using animated cartoons. Health Education Research, 19(5), 591–595. https://doi.org/10.1093/her/cyg079
Moe-Byrne, T., Evans, E., Benhebil, N., & Knapp, P. (2022). The effectiveness of video animations as information tools for patients and the general public: A systematic review. Frontiers in Digital Health, 4, 1010779. https://doi.org/10.3389/fdgth.2022.1010779
Schooley, B., San Nicolas-Rocca, T., & Burkhard, R. (2015). Patient-Provider Communications in Outpatient Clinic Settings: A Clinic-Based Evaluation of Mobile Device and Multimedia Mediated Communications for Patient Education. JMIR mHealth and uHealth, 3(1), e2. https://doi.org/10.2196/mhealth.3732